Lower your Care Compare Readmission and Mortality Statistics
By AccentCareHow an intentional hospice strategy can help your health system improve quality and reduce penalties
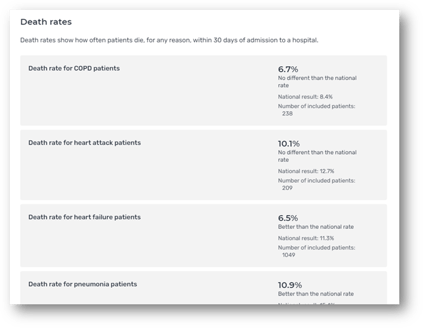
As Hospital Compare has transitioned into Care Compare, more seniors, health plans, and risk-bearing entities are using this Medicare tool to review hospital quality outcomes and data points such as:
-
Readmissions;
-
30-day mortality rates;
-
Benchmarks against other hospitals, and;
-
quality of care provided
This information has never been more accessible to those who are planning for their own care or determining where their patients or attributed lives should go.
Statistics don’t tell the whole story
These rates can be frustrating for hospital providers. There are many different factors that might contribute to readmissions, mortality rates, and differences in quality scores.
Furthermore, the U.S. Department of Health and Human Services (HHS) notes that,
“Value Based Programs should account for differences in populations between providers and, in particular, whether programs should account for beneficiaries with social risk factors—people for whom factors such as income, housing, social support, transportation, and nutrition might adversely affect access to health services or desired health outcomes.” ¹
HHS acknowledges that social determinants of health should be factored into these results, though they currently aren’t. Patients who are dually eligible for Medicare and Medicaid, or those who suffer from food insecurity, lack an adequate social support system, or those who have multiple comorbidities are more likely to be readmitted or die within 30 days of a hospital stay. At first glance, these cases might be uncontrollable, even with the best of discharge plans.
Anticipating the decline of seriously ill patients
While hospitals can’t see around every corner, prognostication is possible. In hospice, professionals often use this question as a quick gut check to determine how a patient is likely to fare:
“Would you be surprised if this patient died in the next six months?”
(final hospice eligibility is determined by two physicians certifying that a patient will die within six months if their disease runs its normal course).
Of course, no physician, nurse, or member of the hospital team can tell precisely when a patient may die. However, many clinicians have experience with patients who cycle through their hospital regularly when it’s clear the patient likely has only months or weeks to live.
Many of these readmissions could be the result of the underutilization of hospice services by Medicare beneficiaries:
- In 2018, barely half (50.7%) of all decedents received hospice before dying
- Of those who received hospice, 40.4% received no more than 14 days of care²
Appropriate hospice referral can improve patient satisfaction and quality scores
Hospice is unique among Medicare benefits- an interdisciplinary team comes together to surround the patient and their family, offering comfort and support far beyond many other care models. Pain control, medication management, and durable medical equipment are all provided. Not only is physical comfort a core aim of hospice, but so are adequate psychosocial counseling, social service support, and even spiritual care. Families of patients also receive 12 months or more of bereavement care, even if their loved one was on service only for a few hours.
What does a timely referral to hospice achieve for a hospital or health system?
- Lower 30-day readmissions: Hospice is designed to provide support for many of the social determinants of health that can keep patients cycling through an emergency room or intensive care unit every few weeks.
- Lower mortality statistics: When an eligible patient transfers to hospice, even if they stay in a hospital receiving hospice general inpatient or respite care, their death is not included in the hospital’s mortality rate.
- Higher patient and family satisfaction: Hospice CAHPS scores are among the highest within Medicare- patients and families report higher overall satisfaction that the hospice interdisciplinary team provides at the end of life.
- Lower hospital staff burnout: Hospital staff can struggle with providing curative care or heroic measures to frail or dying patients. The emotional distress caused by performing CPR on a medically fragile and elderly patient can be significant, as can witnessing the discomfort of an intubation. Knowing that hospice-eligible patients are receiving appropriate care means hospital staff can focus on those who can truly benefit from their curative care.
A thoughtful and strategic hospice partnership can help hospitals provide the care patients need while also helping with key metrics on Care Compare. Working to ensure that your hospice utilization strategy is intentional and effective is a critical component of health system management. No longer can hospice referrals be offered as an afterthought in the last days or even hours of a patient’s life, but they should rather be thought of as a core quality and management strategy for a forward-thinking hospital administration team.
¹ Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health & Human Services. Second Report to Congress on Social Risk Factors and Performance in Medicare’s Value-Based Purchasing Program. 2020. https://aspe.hhs.gov/social-risk-factors-and-medicares-value-basedpurchasing-programs
² NHPCO Facts and Figures 2020

