Providing the Best Care Begins with Acknowledging the Background of Our Patients
By AccentCare Understanding the unique beliefs, traditions, expectations, and desires of the patients and families we serve can make an impact on the care that we provide and the satisfaction that patients experience.
Understanding the unique beliefs, traditions, expectations, and desires of the patients and families we serve can make an impact on the care that we provide and the satisfaction that patients experience.
This often starts with understanding the background of those we serve. The Institute of Medicine’s report “Unequal Treatment” concluded that “racial and ethnic minority patients are found to receive a lower quality and intensity of healthcare and diagnostic services across a wide range of procedures and disease areas.” [1] This can subsequently affect that patient’s satisfaction with the care received.
As healthcare providers that are focused on the best quality outcomes for our patents, one of the ways that you can ensure improved patient satisfaction is when your patients utilize end-of-life planning and care. In fact, data shows that when eligible patients utilize hospice, ACOs, MCOs, and delegated risk providers can increase quality metrics and save money. There is an option for better outcomes for these patients, and it starts with taking a look at the demographics of who is utilizing end-of-life services.
Looking At the Data – Who Receives Hospice Care?
According to National Hospice and Palliative Care Organization’s (NHPCO) 2020 report based on CMS data, 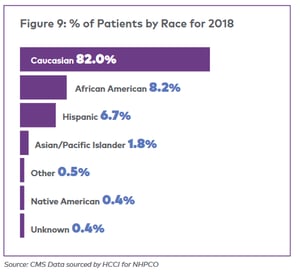 utilization of hospice by race varies significantly. 82% of hospice care is utilized by Caucasians, a figure which does not align with the most recent US Census estimates of the makeup of the United States.
utilization of hospice by race varies significantly. 82% of hospice care is utilized by Caucasians, a figure which does not align with the most recent US Census estimates of the makeup of the United States.
Minority groups are less likely to report having had a discussion around advance directives and end of life planning with their healthcare provider[2], which are often a key part of the decision for patients to consider hospice care. Studies have shown that while cause of death may be similar, both Black and Latinx patients are more likely to die in a hospital and not on hospice than white patients[3], often resulting in increased costs and stress for patients and families.
Discussing end-of-life care and decisions is a difficult topic for most people, but when combined with a history of inequality, misrepresentation, and cultural differences, it’s not hard to understand why these conversations might not be happening frequently.
Change Requires Educating Ourselves Before We Educate Others
Healthcare providers have a responsibility to ensure that patients and families can access the services that they are entitled to, and part of the solution is beginning to address the continuing causes of disparity. Before a trusted healthcare provider begins conversations around end-of-life care, it’s important to understand the key differences in how different populations view things like talking about death and healthcare in the late stages of disease and at end-of-life.
- Identify Who You’re Serving. In order to have the conversation, you need to know who you’re talking to. Start by educating yourself first about potential beliefs, experiences, and preferences of the local populations you provide care for most frequently.
- Starting the Conversation. One of the largest barriers to access is miscommunication and misunderstanding. In some Asian and Latinx cultures, talking about death may be considered disrespectful or off limits.[4] In the Black community, some feel that talking about illness may hasten death.[5] This knowledge can help inform how you approach the conversation. While your patients may trust you, it’s possible that they are uncomfortable addressing certain subjects. How then can we as providers create an opportunity to have honest conversations about serious and illness and death that respect the wishes and boundaries of patient populations?
- Ask Questions and Actively Listen to the Answers. Listening is one of the most important ways we can express cultural sensitivity. While there may be similarities that individuals of a certain population tend to share, each patient and family has their own unique background. Listening to their story, their beliefs, and their fears should inform the way that you approach healthcare conversations with them.
- Don’t Rush the Conversation. Talking about end-of-life care is a weighty issue, especially for those who may not feel comfortable talking about death or who have mistrust in the healthcare system. Give your patients and families space and time, and don’t force immediate decisions. The earlier you can start the conversation, the better. Your hospice partner is there to help when you feel the time is right and the patient and family are open to end-of-life care; when you let your healthcare partners know about the background and values of your patients, they can step in with the knowledge to seamlessly continue the conversation.
- Educating Your Staff. Providing patients with the care they deserve is a team effort. These resources and education materials are appropriate for any healthcare professional to utilize.
- Cultural Humility Chart. This resource lists questions that you can ask your patients and families to facilitate respectful and culturally sensitive conversations about end-of-life issues.
- CE/CME Course: “Cultural Considerations for Supporting Black/African American Patients at the End of Life.” This free course is open to all. RNs, MDs, NPs, PAs, social workers, and long term care administrators can view to earn continuing education credit.
- Article: “Honoring the Legacy of your Black/African American Patients Starts by Asking the Right Questions.” This article demonstrates how to use knowledge about a patient’s background to start asking relevant questions.
Patients and families should be provided with all of the information that can help them make the best decisions for them – and it should be conveyed in a way that recognizes the cultural values and history of the populations we serve.
References:
[1] Unequal Treatment:Confronting Racial and Ethnic Disparities in Health Care
[2] Advance Directive Discussions: Lost in Translation or Lost Opportunities?
[3] Racial and Ethnic Differences in End-Of-Life Costs
[4] Challenges and cultural barriers faced by Asians and Latinos at the end of life
[5] Barriers to End-of-Life Care for African Americans From the Providers’ Perspective: Opportunity for Intervention Development
